Finding new treatments for today & cures for tomorrow
We bring together influential academics and clinicians from across the world, all with a shared passion to understand hearing and a shared goal to cure hearing loss. Our science continues to set best practices with a fully integrated model of clinical and research activities allowing us to translate our knowledge into tangible outcomes for our community and beyond.
We were the first Australian World Health Organization Collaborative Centre for ear and hearing research and education, which has given us the opportunity to increase our impact on the global pandemic of hearing loss.
Over 1.5 billion people currently experience some degree of hearing loss, which could grow to 2.5 billion by 2050. In addition, 1.1 billion young people are at risk of permanent hearing loss from listening to music at loud volumes over prolonged periods of time. The World Report on Hearing shows that evidence-based and cost-effective public health measures can prevent many causes of hearing loss.
We embrace multidisciplinary research and opportunities to collaborate which allows us to develop strong, intellectually diverse teams that can answer complex research questions. Our researchers, audiologists, clinicians, scientists and surgeons all work together to enhance the lives of those with ear and hearing disorders, discovering and delivering innovative treatments.
Our five research areas below focus on developing groundbreaking cures for tomorrow’s generations.
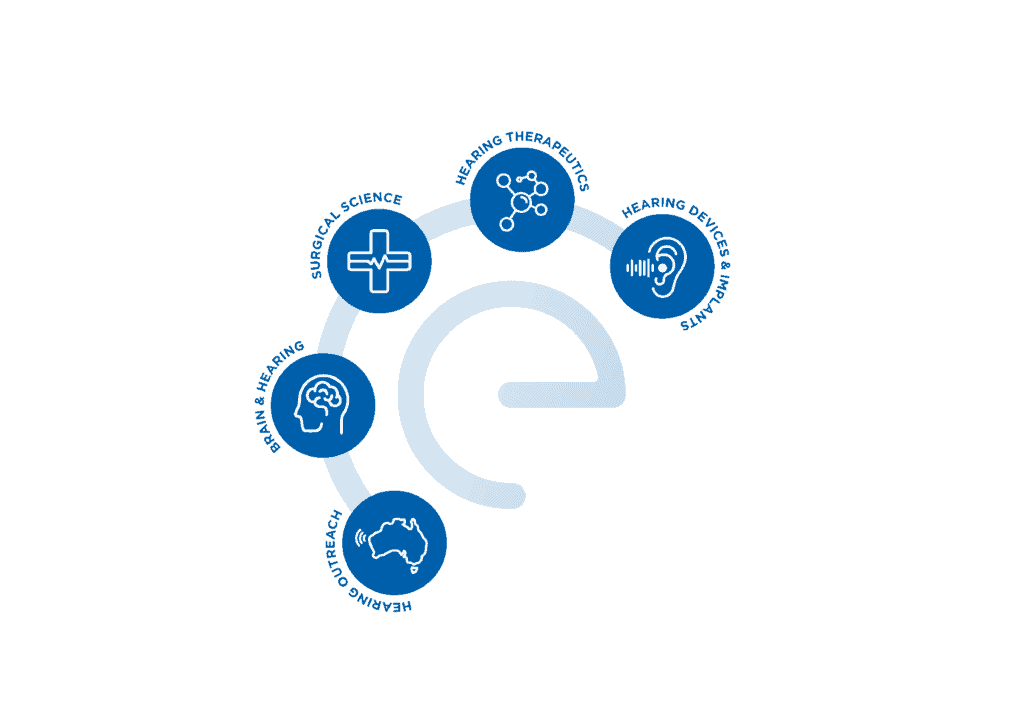
Brain and Hearing

Scientific Lead Adj Assoc. Prof. Dona Jayakody
Our data from the Australian population suggest hearing loss is associated with mental health and cognitive decline. If untreated, hearing loss could impede healthy ageing in older adults, posing a substantial challenge to our healthcare system. Higher priority is being given to prevention, early intervention and non-institutional care. New knowledge is required that can be translated into clinical practice and innovative clinical strategies for people living with hearing loss and its associated challenges.
Current gaps in current research: (i) lack of evidence from Randomised Control Trials (RCT) on the impact of hearing rehabilitation on cognitive function, and mental and psychosocial well-being. (ii) insufficient data on untreated hearing loss and its impact, and barriers to accessing hearing healthcare in Indigenous & Culturally & Linguistically Diverse (CALD) older Australians; (iii) lack of interdisciplinary communication among hearing healthcare professionals, GPs and Gerontologists on how to best support hearing-impaired older adults with/at risk of dementia; and (iv) lack of clinical guidelines, tools and devices suitable for hearing impaired clients with/at risk of dementia.
OUR VISION is to address knowledge gaps through five project areas to facilitate healthy ageing in hearing-impaired seniors with equitable healthcare across communities.
Projects:
RCTs (HearCog & Hearables): impact of hearing rehabilitation on cognitive, mental & psychosocial well-being of hearing-impaired older adults.
Listen Up: barriers to accessing hearing services, the impact of untreated HL & hearing rehabilitation on Indigenous older adults.
Hear2gether: hearing equity for CALD Australian seniors: association between untreated hearing loss, cognition and mental health and barriers to hearing healthcare in CALD older Australians.
Knowledge, Attitudes & Practices (KAP) survey & training for hearing healthcare professionals, gerontologists & general practitioners to support older adults with hearing & cognitive impairment
Commercialisation: objective hearing test & a prototype of a hearing device suitable for hearing-impaired older adults at risk of dementia- industry-funded
Publications:
Jayakody DMP, Friedland PL, Eikelboom RH, Martins RN, Sohrabi HR. A novel study on the association between untreated hearing loss and cognitive functions of older adults: Baseline non-verbal cognitive assessment results. Clin Otolaryngol. 43:182–191; 2018. doi.org/10.1111/coa.12937
Jayakody DMP, Almeida OP, Speelman CP, Bennett RJ, Moyle TC, Yiannos, JM, Friedland PL. Association between speech and high-frequency hearing loss and depression, anxiety and stress in older adults. Maturitas. 110:86-91; 2018. doi:10.1016/j.maturitas.2018.02.002
Jayakody DMP, Friedland PL, Nel E, Martins RN, Atlas MD, Sohrabi HR. Impact of cochlear implantation on cognitive functions of older adults: pilot test results. Otol Neurotol. 38(8):e289-e295; 2017. doi:10.1097/MAO.0000000000001502
Hearing Therapeutics

Scientific Lead | Adj Assoc. Prof. Elaine Wong Clinical Lead | Prof Marcus Atlas
Recent advances in personalised stem cell regenerative medicine and gene therapies have highlighted the potential success of new hearing loss therapies. Given that currently, there are no pharmacological or cellular treatments available for disabling sensorineural hearing loss, our focus on hearing therapeutics provides hope for inner ear tissue repair and regeneration using cellular and pharmacological treatments.
Our Hearing Therapeutics team is collaborating with clinicians at Lions Hearing Clinics, Lions Eye Institute, hospitals and Genetic Services of WA to develop the Australasian Hearing Registry and Biobank (AHRB). The first of its kind in Australia, the Biobank will store tissue related to genetic-associated hearing loss with the goal of advancing personalised care and novel treatments.
Significantly, two-thirds of childhood hearing loss has a genetic cause. The Biobank will allow increased access to genetic samples by linking to national and international registries, helping researchers develop therapies for various types of inherited hearing loss. Over 100 genes have been identified as associated with hearing loss. Gene therapy has the potential to restore hearing in patients with profound genetic hearing loss.
Recent gene therapy trials overseas have shown life-changing results in children who could previously not hear, and we anticipate the biobank facilitating more of this research in Australia.
Projects:
Curing hearing loss:
This gene-based therapeutics research aims to explore two main lines of research enquiries.
The first is the application of genes in hair cells and neural regeneration to treat hearing impairment. The second is using stem cells to generate patient-specific hair cells to recover hearing loss.
The research includes the newly developed patient-specific induced pluripotent stem cell and inner ear organoid model that will allow the exploration of many aspects of inner ear cell biology and cell engineering in the search for a cure for hearing loss.
Targeted drug discovery and delivery for the inner ear:
This program of research is designing new drugs that aim to treat sensorineural, drug-induced, and age-related hearing loss and prevent hearing loss.
The main areas of hearing research include small molecules, and gene and viable cell targeting in the middle and inner ear using bio nanotechnology and pharmaceutical sciences.
Materials to treat eardrum perforation:
Scaffolds and surgical implant research aims to develop commercial end-user devices that can aid damaged eardrums.
With the support of a Wellcome Trust Grant and developed in conjunction with Deakin University, ClearDrum is a prosthetic device designed for those with perforations in the ear drum, which often result from middle ear infections.
This ground-breaking device, which will function as a whole or partial artificial eardrum, may increase the success rate of surgery for patients and optimise healing.
Publications:
DS, Liew LJ, Lye J, Atlas MD, Wong EYM. Overcoming barriers: a review on innovations in drug delivery to the middle and inner ear. Front Pharmacol. 14:1207141; 2023. doi:10.3389/fphar.2023.1207141
Lye J, Delaney DS, Leith FK, Sardesai VS, McLenachan S, Chen FK, Atlas MD, Wong EYM. Recent therapeutic advances in hearing loss. Biomedicines. 11(12):3347; 2023. doi:10.3390/biomedicines11123347
Zaw K, Wong EYM, Zhang X, Zhang D, Chen S, Thompson JA, Lamey T, McLaren T, De Roach JN, Wilton SD, Fletcher S, Mitrpant C, Atlas MD, Chen FK, McLenachan S. Generation of three induced pluripotent stem cell lines from a patient with Usher syndrome caused by biallelic c.949C > A and c.1256G > T mutations in the USH2A gene. Stem Cell Res. 50:102129; 2021. doi.org/10.1016/j.scr.2020.102129
Surgical Science

Clinical Lead | Prof. Marcus Atlas
Research Co-leads | Adj Assoc. Prof. David Sly, Dr. Christo Bester
As we strive to translate research outcomes into clinical practice, close collaboration between scientists and clinicians is critical to research success. This particularly relates to the development of drugs and treatments for middle ear disease and hearing loss, and to cochlear implants.
At Ear Science, we have an environment and structure to support medical practitioners to further their research interests in otology and otolaryngology.
Medical practitioners at all stages of their careers are integrated into our research programs. Medical students, medical residents, those planning or in advanced surgical training in otolaryngology, and ENTs are encouraged to contact one of the clinical/research leads for more information.
Projects:
Fibrosis in the cochlea after electrode insertion: Despite the success of cochlear implantation, there is variability in outcomes which may be attributed to fibrosis (scarring) in the cochlea. An NHMRC-funded collaborative team is examining the extent of fibrosis after electrode insertion, and treatments that may reduce fibrosis.
Outcomes after implantation: Ear Science has one of the largest adult implant programs in Australia, and data are frequently used to report on outcomes after implantation. Topics include asymmetrical hearing loss, tinnitus, quality of life, and service delivery.
Publications:
Braack KJ, Miles T, Amat F, Brown DJ, Atlas MD, Kuthubutheen J, Mulders WHAM, Prêle CM. Using x-ray micro-computed tomography to quantify intracochlear fibrosis after cochlear implantation in a Guinea pig model. Heliyon. 9(9):e19343; 2023. doi:10.1016/j.heliyon.2023.e19343
Sucher CM, Eikelboom RH, Stegeman I, Jayakody DMP, Atlas MD. The effect of hearing loss configuration on cochlear implantation uptake rates: an Australian experience. Int J Audiol. 59(11):828-834; 2020. doi:10.1080/14992027.2020.1768445
Heywood RL, Quick ME, Atlas MD. Long-term audiometric and clinical outcomes Following stapedectomy with the shape memory nitinol stapes prosthesis. Otol Neurotol. 40(2):164-170; 2019. doi:10.1097/MAO.0000000000002069
Hearing Devices & Implants
Scientific Lead | Adj Assoc. Prof. David Sly
Deputy | Dr. Christo Bester
Clinical Lead | Dr. Barbara Heinze
Australia led the world in the development of the bionic ear, the ‘cochlear implant,’ arguably Australia’s most successful medical device. At Ear Science, we are at the forefront of new hearing technologies, in driving the latest development, treatment and care for our patients.
The demand for hearing care devices such as cochlear implants and hearing aids grows as the number of people with disabling hearing loss increases. Audiological and hearing assistance technologies are also converging with smart mobile and consumer audio devices in ‘hearables’ and auditory neurotechnology. We believe we are only at the start of the journey of devices to improve hearing. Ear Science partners with education, industry, and community to develop innovations in hearing devices to improve both diagnostics and treatment in hearing healthcare.
NOTE: Our program is an adult implant program only.
Projects:
New telemedicine hearing tests and devices. Current hearing outreach and uptake of hearing devices is poor. We are developing new hearing tests, devices and digital tools for monitoring and improving hearing care for those in remote Australia and overseas.
Developing new, immersive hearing tests. Standard clinical hearing tests rely on the measurement of pure tones presented via headphones, but this captures only a tiny aspect of the human auditory experience. Here, we are developing new, immersive tests using innovative technological approaches that are based on real world difficulties faced by those with large to small hearing impairments.
New precision tests and devices to better detect and treat hearing loss. Current hearing tests and hearing aids do not localise and target the specific cells related to hearing loss in the inner ear. We are developing more precise device diagnostics and device treatments to address this.
Diagnostics and treatments for hidden hearing loss. Hidden hearing loss is a term for subjective hearing difficulties with clinically normal hearing thresholds. People may hear speech of their loved ones but mishear the details. At present, there is no valid diagnostic or treatment for hidden hearing loss. We are working to develop novel subjective and objective tests, devices, and treatments for hidden hearing loss.
Advanced Cochlear Implant Diagnostics. Cochlear implants are successful treatments for moderate to profound hearing loss. However, an improved understanding of how the body responds to implantation. We are developing advanced diagnostics that will lead to additional improvements in the delivery and post-operative care of implant recipients.
Publications:
Yiannos JM, Bester CW, Zhao C, Gell B, Jayakody DMP. Speech-in-noise performance in objectively determined cochlear implant maps, including the effect of cognitive state. PLoS ONE. 18(6): e0286986; 2023. doi.org/10.1371/journal.pone.0286986
Rance G, Carew P, Winata L, Sale P, Delatycki M, Sly D. Auditory neuropathy in mice and humans with Friedreich ataxia. Ann Clin Transl Neurol. 10(6):953-963; 2023. doi:10.1002/acn3.51777
Brice SB, Sly DJ, Tan SC. Chapter 8. Diagnostics underpinning digital health. In Almond H and Mather C (Eds.) Digital Health: A Transformational Approach. p177-202; 2023. NSW, Australia: Elsevier
Hearing Outreach

Scientific Lead | Adj Professor Rob Eikelboom
Clinical Lead | Dr Anton Hinton-Bayre
Hearing loss is one of the most common global health conditions, affecting about 1.5 billion people. There is a particular burden on people living in developing countries and on Australian Indigenous children and adults.
Ear Science’s Healthy Hearing Outback team has delivered ear and hearing services to the East Pilbara for well over 10 years. Collaborating with the community, strategic partners and funders, the Hearing Outreach and Epidemiology team at Ear Science focuses on developing devices, treatments, and services that will reduce the burden of ear disease and hearing loss.
We are working with the World Health Organization and international partners to better understand and reduce the global burden and risks of ear disease and hearing loss, particularly in the Western Pacific Region.
Projects:
SoundSmiles: This novel app aims to address mental health and hearing loss in Indigenous children. This work is a collaboration with Monash University, Curtin University, South West Aboriginal Medical Service and Puntukurnu Aboriginal Medical Service. Funding from the WA Health-Future Health Research and Innovation Fund.
Ear and Hearing Care in the East Pilbara: To better understand and improve ear and hearing health in the Pilbara, and improve service delivery, we are developing an analysis of 10 years of clinical activity, In collaboration with Puntukurnu Aboriginal Medical Service, WA Country Health Service, Australian Hearing. Funding from Channel 7/Telethon Trust.
The Busselton Healthy Ageing Study. As the population ages it is important to understand how the various aspects of physical and mental health interact with each other, to improve our knowledge of management and treatment of disease. This population study of Baby Boomers focused on changes in hearing over time, and associations with risk factors. In collaboration with Busselton Population Medical Research Institute, and researchers across WA, The Netherlands, and South Africa. Core funding from Ear Science, WA Health-Future Health Research and Innovation Fund.
Publications:
Hunter ML, Knuiman MW, Musk B, Hui J, Murray K, Beilby JP, Hillman DR, Hung J, Newton RU, Bucks RS, Straker L, Walsh JP, Zhu K, Bruce DG, Eikelboom RH, Davis TME, Mackey DA, James AL. Prevalence and patterns of multimorbidity in Australian baby boomers: the Busselton healthy ageing study. BMC Public Health. 21(1):1539; 2021. doi:10.1186/s12889-021-11578-y
Stegeman I, Eikelboom RH, Smit AL, Baguley DM, Bucks RS, Stokroos RJ, Bennett RJ, Tegg-Quinn S, Hunter M, Atlas MD. Tinnitus and its associations with general health, mental health and hearing loss. Prog Brain Res. 262:431-450; 2021. doi:10.1016/bs.pbr.2021.01.023
Tan HE, Lan NSR, Knuiman MW, Divitini ML, Swanepoel DW, Hunter M, Brennan-Jones CG, Hung J, Eikelboom RH, Santa Maria PL. Associations between cardiovascular disease and its risk factors with hearing loss-A cross-sectional analysis. Clin Otolaryngol. 43(1):172-181; 2018. doi:10.1111/coa.12936
_____________________________________________________
Our researchers are affiliated with, and collaborate with the University of Western Australia, and follow the University of Western Australia’s approach to the ANZCCART Openness Agreement on Animal Research and Teaching in Australia.

