Usher Syndrome is an incurable genetic disorder causing hearing loss and visual impairment responsible for over 50% of deafblind people in the world.
There are 3 subtypes of Usher Syndrome which cause different degrees of severity depending on the mutations involved. Severe hearing loss and visual impairment may develop in childhood, early adulthood or even middle age, thoroughly disrupting the lives of those affected.
There is no cure for Usher syndrome and currently treatment for Usher Syndrome-related hearing loss is through hearing aids and cochlear implants. However, research suggests new treatment of gene therapy or cell therapies may offer a cure.
With the support from Channel 7 Telethon Trust, Stan Perron Charitable Foundation and our Gift of Hearing Appeal we have been able to progress the project further to submit the NHMRC Synergy Grant application for $5 million. The proposed funding will be used to support the ongoing Usher syndrome gene therapy pipelines to develop the Australian Usher Syndrome Gene Therapy Coalition which will incorporate strong bedside-bench research pathways with established world leaders in clinical care and scientific research to establish a disease modelling and drug screening platform suitable for the pre-clinical evaluation of treatments for Usher syndrome.
We are working with the retinal specialist Professor Fred Chen, Senior scientists Dr Livia Carvalho and Dr Samuel McLenachan at Lions Eye Institute, Professor Steve Wilton and Professor Sue Fletcher from Murdoch University to understand how Usher affects eyes and ears, and to try to find common methods to correct the defects. This collaboration provides great economy of effort for our Usher research program and new ideas come from the different perspectives each partner brings. In our current research we are investigating how to make cells of the inner ear from Usher patient stem cells. If the stem cells can be turned into the hearing cells that are missing in Usher patients, we may be able to correct the mutation and put the corrected cells back into the patient’s cochlea to restore hearing. In other words, by changing stem cells so they become the cell type in the ear that detects sounds and then implanting these cells into the inner ear, we hope to restore hearing in Usher syndrome patients. Using this same process Prof Chen will put cells back into the retina and restore sight. This approach is reliant on the ability to model the correct cell type and this represents a major effort for inner ear cell biology in our lab. A robust cell model will allow us to explore many aspects of inner ear cell biology and cell/tissue engineering in the search for a cure for Usher Syndrome.
The genetic makeup of patients is also being investigated so that we can develop induced pluripotent stem cell based models from the various mutations that occur in these Usher patients.
Following the development of these key stem cells, we will explore a number of therapies with the aim to replicate the cells of the inner ear.
Our discoveries so far
In the past year we have generated data to support the submission of a patent describing a novel method for generating inner ear hair cells from human skin. We have successfully generated induced pluripotent stem cells (iPSCs) from skin samples of patients with Ushers and have used these human iPSC to generated inner ear organoids. These organoids contain hair cells, the key sensory cells of the auditory system. We are using inner ear organoid cell cultures to evaluate how three common Usher gene mutations – Usher Type I MYO7A, PCDH15 and Type II USH2A – affect hair cell development and function. Our studies have identified the causative gene mutation for hearing loss in Usher patients. In addition, we have identified disease mechanisms and screening potential therapeutics.
These human specific inner ear models have been instrumental in understanding the regulatory pathways required for hair cell development and function and have provided key insights into the biological mechanisms. Our final goal is to differentiate patient-derived iPSCs into inner ear organoids in order to generate a human disease model of Usher syndrome. The disease model will be used for drug testing and therapeutic application.
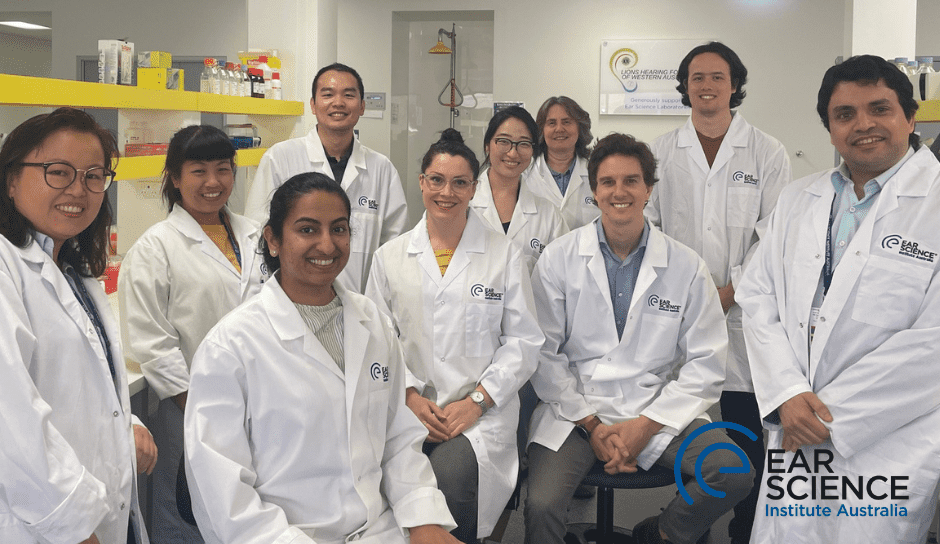
Dr Elaine Wong leads and oversees a stem cell research team, coordinates with research staff and students to work on project aims and ensures timely accomplishment and communication of results. In addition to the support of existing team members, we have recently recruited Ms Varda Sardesai as a research assistant with substantial stem cell working experience in human heart culture from Sydney and travelled to Perth to work at our laboratory on the QEII grounds, as a direct result of your support.
With your support for our Gift of Hearing Appeal we have been able to progress the project further to submit the NHMRC Synergy Grant application for $5 million. The proposed funding will be used to support the ongoing Usher syndrome gene therapy pipelines to develop the Australian Usher Syndrome Gene Therapy Coalition which will incorporate strong bedside-bench research pathways with established world leaders in clinical care and scientific research to establish a disease modelling and drug screening platform suitable for the pre-clinical evaluation of treatments for Usher syndrome.
We have completed Phase I and II and proceeded to Phase III of the Usher research project
Phase I
Usher patient skin tissue collection from 26 patients with Usher syndrome – to characterize hearing phenotypes of Usher patients, identify the Usher gene mutation for Usher patients and establish patient-specific skin fibroblasts cell lines.
Phase II
Usher patient cellular models from 2 patients with Usher Type I MYO7A mutation, 3 patients with PCDH15 mutation and 5 patients with Type II USH2A mutation – to generate Usher patient specific induced pluripotent stem cells and inner ear organoid culture for identifying disease mechanism.
Phase III
Gene therapy for Usher syndrome – 1. to identify pathogenic mechanisms of Usher syndrome and 2. To use this information to test and develop gene therapy approaches, such as gene correction by CRISPR and Antisense oligo nucleotide ASON treatment.