In this episode, Founding Director of Ear Science Institute Australia, Professor Atlas will unpack the latest research in curing hearing loss and what the future might hold.
But how long do we wait for a cure?
Dan van der Meer: [ 00:02This is the Ear Science Podcast, The Science of Healthy Hearing.
Lize Coetzee: [0:08] Hello and Welcome to Season One of the Ear Science Podcast, The Science of Healthy Hearing, proudly presented by Ear Science Institute Australia a not for profit Medical Research Institute. In this podcast, we’ll bring you into our world, the world of Ear and Hearing science. Together with Professor Marcus Atlas. We will discuss the latest in Ear and Hearing Research and what it means to you.
Dan: [0:32] I’m Dan Vandermeer. I’m a digital content specialist and podcast host and passionate about raising awareness for the impact of hearing loss.
Lize: [0:40] And I’m Lize Coetzee. I’m a qualified audiologist and the Chief Operating Officer at Ear Science Institute Australia.
Dan: [0:47] This podcast provides information of a general nature and does not constitute medical advice.
Lize: [0:52] Today we are talking to Professor Marcus Atlas. He’s a surgeon-scientist and the founding director of Ear Science Institute Australia. We’re excited to chat with Professor Atlas for the very first episode of our podcast, and we will discuss the holy grail of finding a cure for hearing loss.
Dan: [1:09] Professor Atlas, welcome to the Ear Science Podcast, The science of healthy hearing.
Professor Marcus Atlas: [1:13] Good Dan, how are you?
Dan: [1:15] Very good, thank you for joining us.
Marcus [1:16] It’s a pleasure.
Dan: [1:17] Now Professor Atlas, I know that I took my hearing for granted, and as a 48-year-old man it’s starting to play effects on me. I played in bands for years in loud rock venues and drums, guitars, and my bad singing all contributed to what I think now, generally, mainly in pubs I have trouble with what we used to call in the music game the muddled mix. I struggle hearing distinct conversations sometimes where noise-ambient noise is quite loud.
Marcus [1:45] Dan, I didn’t know this was gonna be consultation. I can say honestly, you got a few problems.
Dan: [1:51] What do you think our listeners need to know about their hearing in general?
Marcus [1:57] Well, hearing is a really important sense. And it’s what we’ve concentrated on here at Ear Science Institute Australia for over 20 years. And we think that the right of hearing loss and the increase over the years is a real problem in our community. So we set about 20 years ago, doing a whole lot of things to try and help people in Western Australia, nationally, and around the world with hearing loss. And we set about doing it by connecting our clinics, our research and our education altogether. And then it got to the community and we started working on helping people within the community and starting our outreach programs, and Liza will tell you about some of those. But really, it’s a multi dimensional beast. And it’s grown enormously. And I’m really proud of the impact we’ve had within the community, particularly our clinics.
Lize: [2:54] So Marcus, as an audiologist, for me, it is such a unique model, with education, the research and the clinical service delivery working together, can you tell us what the prevalence of hearing loss is and really the impact of hearing loss on people’s quality of life?
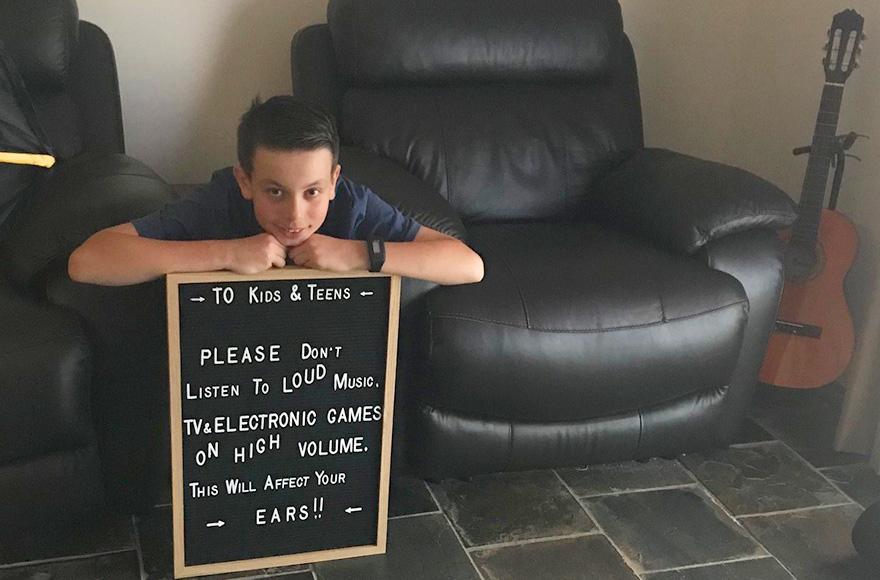
Marcus [3:11] Well, one in six people experience hearing loss and one in four over 65. But by 2030, the number will be even greater. And what we’re starting to see is the two ends. We’re starting to see this increasing number of people who are older, who are living longer, getting more hearing loss and requiring more care. So of course, they require all of our normal interventions, including the use of hearing aids, but many of them are getting to implantable devices like cochlear implants now, because they’re living so much longer. And then there’s Dan’s mates, the ones who are younger, who are exposing themselves to too much noise. And so the way they can experience sound now is different to what I remember when I was a kid. And so they can get a huge amount of volume into their ears easily and our job is to try and protect them from that. So trying to tell the story about being careful, not stopping music, we love music. We all love it. And it’s fun for when it’s loud. But we need to be careful about how much noise exposure and how we tell that age group about how to be reasonable about noise exposure. So there’s these two ends.
Lize: [4:23] That’s sort of that education side and then service delivery. We want to get to people early and educate them on the importance of looking after their ears.
Marcus [4:31] Yeah, we do and that’s one of our jobs. And you and I are out there every day helping patients with hearing loss, but one of our other jobs is to tell this story. That’s what this podcast is doing. Telling this important story of trying to stop people from coming to see us so that we never have to see them because they don’t have hearing loss like the previous generation. So we’re seeing kids, kids who are really young with tinnitus and hearing loss because of noise.
Dan: [5:00] That’s pretty scary.
Lize: [5:02] It’s the hearing loss Marcus, but it’s also the impact that hearing loss has on people. So we know now hearing loss is linked to social isolation, to loneliness, and even cognitive decline. And we hope to hear about these things more in later podcasts with our researchers.
Marcus: [5:22] Lize, thanks for reminding me as always, you remind me most days of things that I’ve forgotten. And it’s the story of hearing loss, isn’t it? It’s what goes on in the background of quality of life and loneliness. But this interesting work that Donner I guess is going to talk to you about Donna Jayakody. And the work she’s done with here, the connection of hearing loss and dementia. So dementia’s really touched my family’s life. And so I’m really aware of what it can do to families like ours and my parents. And hearing loss is one of the things that we can do something about, there’s not so much we can do about dementia at the moment. But there are certain things that we can do to try to prevent, that we know will have a significant impact on the development of cognitive decline. And one of them, the biggest one, believe it or not, the biggest one, is hearing loss in middle age. And that’s what we’re out to do something about, but Donna’s gonna do the unnecessary work that scientists have to do and we have to prove it. We have to prove that if we intervene with hearing aids, particularly that’s her study, that we will slow or maybe even prevent the onset of dementia and how wonderful that will be. So she’s she’s doing that work. She’s doing that wonderful work.
Lize: [6:37] Okay, Marcus, we know you have been at the forefront of ear and hearing surgery for over 20 years, have you seen the way hearing loss has tried to evolve over this time?
Marcus: [6:49] Yeah, I’ve seen things change enormously during my surgical career. What I think I’ve noticed the most in surgery is the progression of implantable hearing devices. That’s just taken my practice over. So when I first started out, it was much more about tumors of the ear, chronic ear disease, some of the hearing reconstruction for a disorder called otosclerosis with stapedectomy, and cochlear implants were in their infancy, and Graham Clark in Melbourne was just beginning to really implement this groundbreaking work that he and others had done in the area of cochlear implantation. So, during my career, it has just blossomed. So there’s been newer devices, changes in cochlear implants, more and more people are now suitable for cochlear implants that were never before. It began in adults and then it started. And then kids are in big group of cochlear implants. And now, of course, as I just told you before, they’re all of these older patients. So we’re seeing the majority of our growth in our implant clinic is in patients over 60. And oldest patients, I think, over 100 Now, and we’ve implanted patients in their 90s, who would have ever thought we would do something like that? So these incredibly independent, particularly women, who are living over the age of 90, who were hearing loss as their primary disability, and they get an implant. So and it works. It works. So there’s 90 year old brain, cops this implant and it works. So it’s remarkable.
Lize: [8:22] And that’s such an important point because there’s still so many people that think cochlear implants are for children only. So that age is no barrier when it comes to to hearing implants. So that is such an excellent point.
Dan: [8:36] And so we’re seeing it all here at Ear Science, it really means a lot to us, this implantable hearing program. They’re hard to run out. So it’s really hard to run an implantable hearing aid program that’s not incredibly well renumerated for the clinicians and administrators that we spend so much time on it. But it’s so important to us at Ear Science Institute, because it has such a big impact. And so we’ve worked really hard to become a really large implant group within Australia. We’re really proud of the work we’ve done. So we’ll see more of that as time goes on, I think.
Lize: [9:11] And we know it’s still 90% of people that need a cochlear implant don’t have one.
Marcus: [9:16] So it’s pretty unbelievable. There are all these people out there who have got severe to profound hearing loss, or types of hearing loss that would be more suited to an implantable device, mainly a cochlear implant than a conventional hearing aid or what they’re doing, and some of them have no hearing aid at all. And so so it’s it’s an a massive group of people in our community that could be helped, I think.
Dan: [9:39] So of course, if they’re engaging in this podcast through YouTube and captions, and they’re reading this they could certainly get in contact and do something about their hearing.
Marcus: [9:47] They could then, and that’s really important because that’s for some of our patients’ captions are really incredibly important. They need visual cues, of course, to be able to communicate and this podcast that we’re all listening to can be really hard for some of the patients with severe to profound hearing loss. And so we can do things to help them. So if they’re if they’re using captions now, they should speak to us we can help.
Lize: [10:10] And I like what you say to get in contact with us. People sort of feel that they need to go and see their GP or the audiologist to come and talk to us about a cochlear implant, but really just contact us and we can take you through that journey. So you can be sort of the leader in your hearing journey. And it’s something that we call patient-centred care, or client-centred care, you are at the center of the care that you receive.
Dan: [10:39]
And you’ve got to take responsibility for your own actions as an adult. So, if you are experiencing those issues, then yes, certainly, it’s time to reach out. So Marcus, putting it quite bluntly, are we ever going to cure hearing loss?
Marcus: [10:53] Yeah, I think that is a really good question. It’s something that I think about every day and I have for a long period of time, since I sort of became involved in the science, so I became a surgeon science. So I was trying to be a surgeon about training to be a medical practitioner means you have to be really aware of science, but we tend to get involved in our clinical work. And I guess, around 30 years ago, I wanted to connect again to science and become a surgeon scientists to connect science and my clinical work, to see whether it was possible to do new things that would help millions of people instead of one person at a time. And so some of the fantastic work that we’ve done over the years here, about trying to cure hearing loss has really come to an important stage. And that’s been because we’ve got a wonderful board and executive who look around the world for the very best people that we can find, to seduce to come to Perth, or maybe we can work with them, whilst they are still wherever they are in the world, and create virtual science, or bring them here to Perth, as I said. And one of them is Elaine Wong, who came from Hong Kong. And her interest is in creating these things called organoids. An organoids is using a stem cell approach, training the stem cell with very special cues and medications and proteins to train the stem cell to become an ear, an inner ear. So she turns this stem cell and over a period of time, over months, to become a human three dimensional inner ear, the organ of hearing the cochlea. And so inside that has got these tiny little hair cells, which are the endpoints of nerves, and they’re the ones that pick up the sound and connect up to the brain via nerves. And this organoid is the organ of hearing the cochlea. So it looks actually a little bit like the human inner ear cochlea, which is like a snail, it looks like a snail shape, that’s what the cochlea is, and inside these special hair cells, and she’s been able to grow these organoids that actually have these hair cells that start to form into a sort of snail shape, and connect up to these nerve fibers starting from a single skin cell that becomes a stem cell. And it is programmed with the genes that the cell that it came from, so your skin cell will become your cochlea. And so she grows your cochlea, it’s just unbelievable. She grows your cochlea, and then she can do some experiments with it. So she can look at spatial pathways or particular medications, and try to see what goes wrong with certain types of genetic hearing losses, particularly Asha syndrome, which is a real big interest of ours here. But other causes of hearing loss so that she can devise experiments and medications and treatments and genetics, that might be able to modify the process that cause hearing loss. So this is really something that will make a difference. So this is the organoids story and the way we’re using organoids, it’s not so much the organoid itself. We’re not particularly thinking of could we, everybody asked, could you transplant my organoid back into my ear to make a new cochlea because mine’s mine stuffed up from some other cause? Well, that won’t be easy. So we’re looking at other ways, can we use the organoid to devise ways that we can deliver drugs, proteins, genes to the inner ear to cure the hearing loss? And so that is been an incredible change in the way we do things because we now have got a human model rather than an animal model for hearing loss and the way we might be able to modify it. So now we’re starting to use these organoids on this disorder called ototoxicity. And ototoxicity is drugs particularly and in this case drugs that treat cancer, that are toxic to the inner ear. So what they do is they paralyze or damage the inner ear hair cells, because that’s a side effect of the drug. But the drug is primarily aimed at trying to kill the cancer cells, but they also killed it in the ear. So patients get hearing loss, and some of them get severe hearing loss, and some of the get more minor hearing loss. And these are particularly drugs that are used in childhood cancers. So these are kids who develop hearing loss from the from these medications, this ototoxicity. And of course, they keep that hearing loss for the rest of their life. So what can we do to prevent this ototoxicity and Hanieh Salami is a pharmacist by training, who’s a scientist who works in our lab, another fantastic recruit into aEar Science Institute Australia here in Perth, where he will look at, and he is looking at particular drugs that will antagonize this ototoxic effect. And he’s using the organoids to experiment on that. So this is some of the first forays into the prevention of hearing loss by the use of these organoids.
Lize: [16:03] And they will have such a massive impact on these children’s lives.
Marcus: [16:08] Yeah, some of them would require hearing aids, some of them would require potentially cochlear implants from their ototoxicity. So imagine being able to prevent it, it would be such a wonderful thing for these kids.
Lize: [16:19] So, Marcus, it’s amazing the amount of research that’s happening currently in our labs, how was this research funded? And where is it done?
Marcus: [16:29] Yeah, researching is a tough thing to fund, let me tell you, and the funding comes from various sources, both for infrastructure and buildings, as well as people. And it comes from government agencies like the National Health and Medical Research Council, the Australian Research Council, so they’re government, national government funding groups, there’s state funding groups, they’re not as large as the national groups. There’s philanthropy. There’s non-government organizations. So you can imagine our scientists are spending their entire time searching out grants, which are really hard to get. It’s hard being a scientist in Australia, and being able to find funding. But for our infrastructure we are very, very lucky that there are philanthropists here in Perth, who have been incredibly generous to our Ear Science Institute Australia, our building here in Subiaco, has been funded primarily by philanthropy, and our research building, where we’re now got a floor of 600 square meters of basic science area that’s dedicated completely to Ear and Hearing science, and that’s a big amount of science space in the world. And that’s funded by philanthropy. That’s the Reverend Patricia Surridge family philanthropy, for which we’re incredibly grateful and We occupy part of that building. So you can see it sort of comes from various sources.
Lize: [17:55] Yeah, fantastic. So Marcus, we’ve spoken about what we would call nerve hearing loss or hearing loss in the hearing organ, but I know middle ear infections is another big problem for our children. I was privileged enough to visit the Pilbara and the Aboriginal communities there. And it was just so evident, there are so many Aboriginal kids currently, that are not getting the education that they need, because their ears are infected. What are we currently doing in that space to help middle ear infections and even the the long lasting effects of middle ear infections? And we talked about perforations.
Marcus: [18:35] Well, indigenous ear disease is a is a terrible blight on our society. My whole career, indigenous ear disease has been really the worst part of middle ear disease in Australia. It’s just unbelievable that in our world, our incredibly well off nation has Indigenous kids who have just have this blight of middle ear disease. And despite all of the efforts of a lot of people over the years, it’s still continuing and a terrible problem. But there is much interesting work that science can do to try and help. And so we’re actually a world leading group, probably the world learning group in the understanding of the eardrum. So the human ear drums made out of three layers, a middle layer, that’s part of the middle ear lining, a Middle fibrous layer and the outer layer, which is made of a special type of skin. And so we’ve been working on understanding the skin layer so that we could develop this thing called Clear drum, and clear drum is a work that we’ve been doing for 20 years, which is a scaffold made out primarily out of silk. So believe it or not, we actually using silk, like the textile silk, which has got a biological application. And so we use it in the body and it’s been used. You’ve heard of silk sutures. So you sutures that set up the skin. And it’s the same sort type of silk but actually made into other membrane. So it starts from the silkworm, and ends up as this transparent membrane that we use for clear drum, which is the reconstruction of the eardrum. And from this work that we’ve done on the eardrum, we’ve been able to develop this group of scientists who have this incredible understanding of middle ear disease, and particularly how we’re going to treat it. So clear drum is about repairing the eardrum, which is a big problem in Indigenous kids, but it’s also a problem in non Indigenous Australians. And how we are going to utilize clear drum for repair of the eardrum, but also how we’re going to modify the middle ear disease, the infections they get of the middle ear and mastoid bone. And that’s our next layer of work about how we’re going to understand that how we’re going to use drug therapy, how we’re going to use new approaches to this middle ear disease. So we hope that we’ll be able to imply that to Indigenous Australians, particularly kids, to be able to prevent the onset of middle ear disease and the associated hearing loss, and educational and other quality of life problems that happen in this community that we would really like to improve. And so you know, this has an enormous impact on the way they live in civic life, the job seeking, education, it’s just this massive impact. And so if we can get to the bottom of it, it’s probably not just the eardrum, there’s a lot of other factors that lead to lead to middle ear disease. And there’s work that’s being done around our country to try and understand better why Indigenous kids get more middle ear disease than their non Indigenous Australians, but they do, terribly. And so to understand the why, and to be able to treat it more effectively, would make them, as you say, a massive impact, massive on education, and an opportunity.
Lize: [21:57] And at Ear Science, I feel we really approaching it really well. We both deliver services in the Pilbara to the community. But we also tackling from a science perspective to see how we can, treat these children, how we can treat the ear disease differently, and not just continuing to test hearing day in and day out. Because we need to change how things.
Marcus: [22:22] I think there’s a lot of things that have been done over the years, and I’ve been part of that that have been repetitive and unsuccessful. And just doing the same thing again, and expecting a different outcome is not smart.
Lize: [22:35] And really how we tackle everything that we do. Bringing the research and clinical care together we do that at Lions Hearing Clinic, everything is informed by science, it’s evidence based. The problems we see in clinic, we also feedback into research to make sure that what the researchers are doing, are actually informed by what clients and patients are currently struggling with. So that’s very exciting. So Marcus, as an audiologist working in Lions, we always get asked, is there a cure for hearing loss and should I wait? So you touched on sort of the work we’re doing at Ear Science, but can you tell me what do we say to our clients? Is there a cure and should I wait?
Marcus: [23:16] We’ll say that there will become a cure, but don’t wait. And so the kind of things that we’re doing now, in terms of hearing aid technology and implantable hearing devices, is just unbelievable. And so to deprive yourself of access to those wonderful things at the Lions Hearing Clinics would be crazy. We can do things, that doesn’t mean you will miss out on a potential cure for hearing loss in the future. So even if we put a cochlear implant in place, it doesn’t mean that some of the things that I’ve described to you today won’t be available to you. So that’s the first thing. You can have a hearing aid and improve your quality of life within days of seeing an audiologist at Lions Hearing Clinic and it will transform the way you deal with your family and the way you deal with your friends. And then what you do at work, it will just you will be transformed by the fitting of a hearing aid with hearing loss. So don’t wait. I think the Lions Hearing Clinic laser might see 35,000 people in a year, that’s just unbelievable what you’ve created. And so if all of those people were to miss out on this wonderful opportunity to hear hear again, it would be a terrible shame. So they should not wait for hearing for a cure. But they will be one and they should be involved in it. They should be interested in it. They should become trial participants if they ever get the opportunity and to stay part of it but make sure that they stay part of the hearing world to be able to communicate with their friends and family I think.
Lize: [24:46] So Marcus, this is a podcast for the community. For people in Perth and around the world. How can how can they get involved in finding a cure for hearing loss?
Marcus: [24:59] Well, they can join Justin Langer, who of course, is the Australian cricket coach and he’s also the healthy hearing ambassador for Ear Science Institute Australia. They can become just like him and become an ambassador for us here and tell the story of hearing loss, and become part of understanding and telling the story about hearing health in our community. They could become involved, they could become involved in a clinical trial. That will happen, Donna’s recruiting at the moment. There’ll be future clinical trials, clinical trials they might want to become involved in. They could become involved in philanthropy. So there are hundreds of West Australians that are involved in donating to a gift of hearing, which is aimed in trying to do exactly what we talked about today, to try and improve the lives of people with hearing loss. So there’s lots of ways our community can get involved here at Ear Science.
Lize: [25:57] And everybody that sees us, that he assigns at Lions Hearing Clinic is really part of finding a cure for hearing loss.
Dan: [26:03] Professor Marcus Atlas, this has been so interesting and inspiring. Thank you, the future is looking very bright. What are the three key things that you want our listening audience, the people listening to this, and rating this podcast to takeaway from what we’ve talked about today?
Marcus: [26:18] Well, thanks Dan, for being here. Again, it’s wonderful to have you at Ear Science and and becoming part of everything we do. So there are three take home messages, I think. A cure for hearing won’t happen overnight, so don’t ignore hearing loss, come to Lions Hearing Clinics, get your hearing checked, and this will be a really important part of your life in the future. The second thing is the work in our lab is incredibly promising. And we know that we’re one step closer to this cure for hearing loss. And the third takeaway message is that you can help us, and you can help us by becoming involved in the ways that I’ve talked about in Ear Science, and particularly donating to our gift of hearing campaign, and helping all of the people that have hearing loss and all of the ways we’re trying to improve their life.
Dan: [27:12] Professor Marcus Atlas, thank you so much for joining us today.
Marcus: [27:16] It’s a pleasure Dan, thanks for being with us.
Lize: [27:18] Thank you so much. Can you imagine personally being part of finding a cure for hearing loss? over 20 years ago, Professor Marcus Atlas began the journey of Ear Science Institute Australia, making hearing a focal point for our local community. Professor Atlas had a dream. He wanted to bring world class research, surgery and audiology to people of Western Australia. Fast forward to July, and the importance of hearing loss is being recognized on a global stage. In 2019, the Institute was appointed as one of only six designated World Health Organization collaborating centers for Ear and Hearing Care. We have brought together a team of over 150 surgeons, researchers, medical specialists, scientists, audiologists and support staff. We are proudly at the forefront of internationally recognized research, providing word leading education and shining a light on the importance of untreated hearing loss in our community, all from Perth in Western Australia. You can join us in finding a cure, head to www.earscience.org.au. Click on donate to find out how your support can make a difference to save many lives.
Dan: [28:42] If you’ve enjoyed this episode, let us know by rating and reviewing this podcast or sharing it with a friend or family member. Make sure you subscribe so you don’t miss an episode. Next time we will be talking to Dr. Beck Bennett, an audiologist and researcher who will share her insight into the social and emotional impacts of hearing loss.
Lady: [28:59] Hearing is about communication or the importance of hearing losses because of how it affects communication. And so I would say Good communication is everyone’s responsibility.
Dan: [29:10] To view this episode with captions, visit the Ear Science YouTube channel or our website www.earscience.org.au/podcast to suggest a topic for a future episode links to more information and all the research papers on this topic, visit our website www.earscience.org.au/podcast. The producer of the Ear Science Podcast The Science of Healthy Hearing is Emma Eiland with sound engineering and editing by myself Daniel Van Der Meer. We acknowledge the traditional custodians of the land we’re recording this podcast on, the Whadjuk people of the Noongar nation and land on which you’re listening from. We pay our respects to Aboriginal elders past, present and emerging.